Oral Presentation The Annual Scientific Meeting of the Endocrine Society of Australia and the Society for Reproductive Biology 2014
Ipilimumab-induced hypophysitis in patients with metastatic melanoma: A novel form of autoimmune pituitary disease (#202)
Introduction:The novel fully human monoclonal antibody Ipilimumab (Yervoy: Bristol-Myers Squibb) is an anti-cytotoxic T-lymphocyte antigen-4 (CTLA-4) therapy which disrupts immune tolerance to antigens located on tumour cells. Ipilimumab confers significant survival benefit & prolonged stable disease in metastatic melanoma however is associated with several endocrinopathies, presumed autoimmune, including thyroid dysfunction & adrenal insufficiency (primary & secondary). Hypophysitis, a previously rare disease, appears to be the most common Ipilimumab associated endocrinopathy, with reported incidence of 0-17%1.
Methods:All patients were evaluated at the Chris O’Brien Lifehouse Cancer Centre & Department of Endocrinology, Royal Prince Alfred Hospital or Crown Princess Mary Cancer Centre & Department of Endocrinology, Westmead Hospital between 2012-2014. Relevant data was extracted by review of medical records.
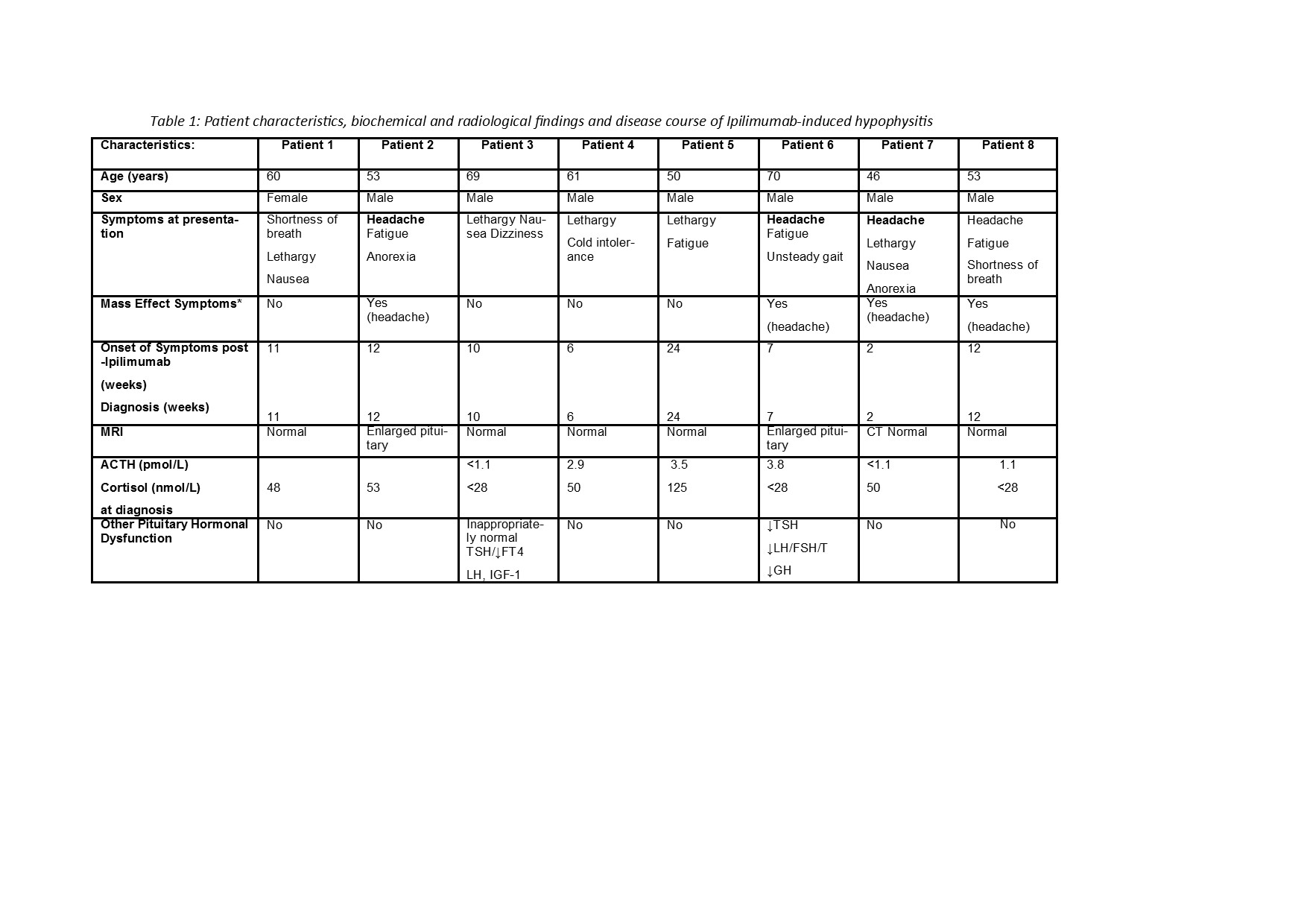
Results:Patient characteristics, biochemical & radiological findings & treatment course pertaining to Ipilimumab-induced hypophysitis are summarised in Table 1. Secondary hypoadrenalism was confirmed via baseline early morning ACTH and cortisol levels with dynamic testing if indicated. Our case series of 8 patients demonstrated variable onset of hypophysitis 2-24 weeks post-initiation of Ipilimumab therapy. Clinical presentation was generally non-specific, with only 4 patients presenting with headache. Diagnosis was confounded by concurrent glucocorticoid therapy in 1 patient. Panhypopituitarism occurred in 2 patients. In contrast to previous reports2, hypophysitis was not generally associated with disease responsiveness during Ipilimumab therapy.
Conclusion:In our case series of 8 patients with metastatic melanoma, hypophysitis occurred as early as 2 weeks & as late as 6 months post-initiation of Ipilimumab therapy. All continue on maintenance glucocorticoid replacement with no evidence of reversibility. These results highlight the importance of baseline hormonal screening & continued surveillance, as a high index of clinical suspicion is essential to prevent delayed diagnosis & associated morbidity.