Oral Presentation The Annual Scientific Meeting of the Endocrine Society of Australia and the Society for Reproductive Biology 2014
Effect of therapeutic glucocorticoids on insulin sensitivity, cardiovascular risk and energy metabolism in patients with inflammatory arthritis (#114)
Insulin resistance can increase arterial stiffness acutely by reducing endothelial function and chronically by stimulating atherogenesis. Postprandial glucose is more strongly associated with vascular dysfunction than fasting glucose concentration. Low dose prednisolone causes insulin resistance and postprandial hyperglycaemia. We investigated whether prednisolone-induced insulin resistance is associated with postprandial vascular dysfunction. Our secondary aim was to investigate the effect of prednisolone on postprandial fat oxidation.
Eighteen subjects with inflammatory arthritis (6 males, age 63.9±7.3 years, BMI 28.1±5.2kg/m2) who had not taken oral glucocorticoids for ≥6 months were studied before and after prednisolone 6 mg/day for 7 days to determine the acute effect of prednisolone. Pre-prednisolone data were also compared to 18 subjects (6 males, age 66.2±6.8 years, BMI 27.9±6.1 kg/m2) taking long-term (>6 months) prednisolone (6.5±1.8 mg/day) to determine the chronic effect of prednisolone. Arterial stiffness (augmentation index measured by applanation tonometry), endothelial function (reactive hyperaemia index by peripheral artery tonometry) and fat oxidation (by indirect calorimetry) were measured before and after a mixed meal (10 kcal/kg, 45% carbohydrate, 15% protein, 40% fat). Insulin sensitivity was estimated using the Matsuda index.
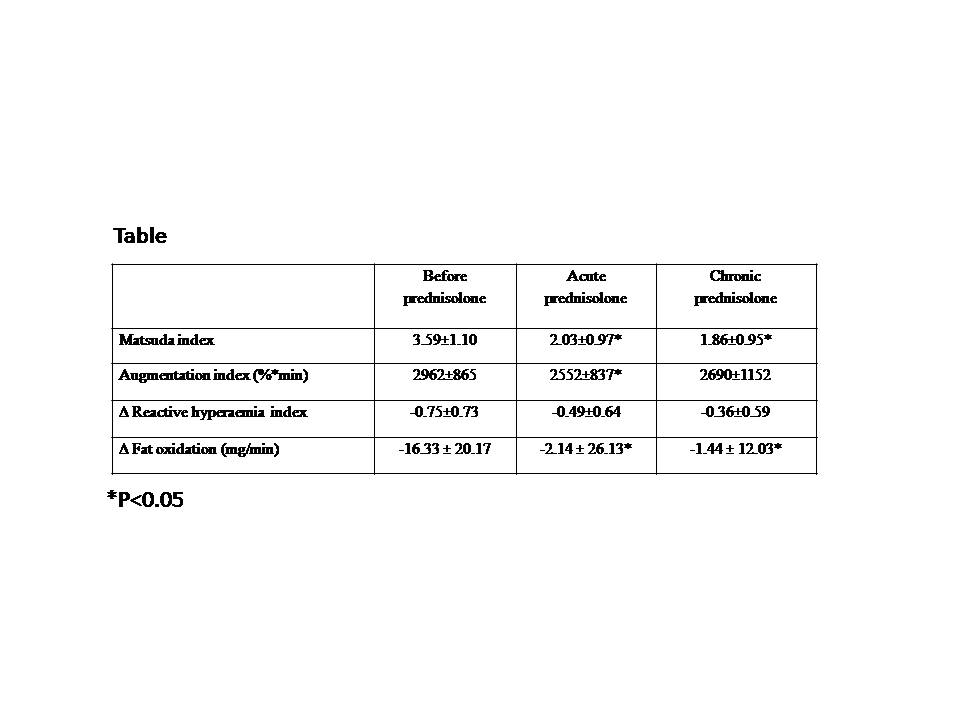
Insulin sensitivity was reduced by acute (p=0.01) and chronic (p=0.04) prednisolone (Table). Postprandial augmentation index was lower after acute prednisolone (p ≤0.001) indicating reduced arterial stiffness, but not during chronic prednisolone use (Table). The postprandial reduction in reactive hyperaemia index did not change with acute prednisolone, but tended to be lesser in patients on chronic prednisolone, suggesting increased postprandial endothelial function (p=0.09) (Table). Both acute (p=0.01) and chronic (p=0.01) prednisolone attenuated postprandial suppression of fat oxidation (Table).
In conclusion, acute and chronic low dose prednisolone reduced insulin sensitivity. However, this was not associated with adverse changes in vascular function. Fat oxidation did not suppress postprandially in subjects on prednisolone, which may be secondary to but also exacerbate insulin resistance.