Poster Presentation The Annual Scientific Meeting of the Endocrine Society of Australia and the Society for Reproductive Biology 2014
Cushing’s conundrum: A case of Primary Pigmented Nodular Adrenal Disease in a 60 year female (#234)
A 60year old female with difficult to control hypertension and poorly controlled type2 diabetes was referred for investigation of hypercortisolism. She had multiple comorbidities including COPD requiring treatment with inhaled corticosteroids. Clinical examination revealed a BMI of 31, supine hypertension (BP 160/90), truncal obesity, proximal muscle wasting and weakness but no evidence of striae, bruising, skin thinning or buffalo hump. She was not pigmented, had no abdominal masses and had normal visual fields.
Investigations for secondary hypertension showed a normal aldosterone to renin ratio 18.6 (n<20), plasma metadrenaline 139pmol/L (n <500pmol/L) and normetadrenaline 92 pmol/L (n <90 pmol/L). GH, IGF-1, thyroid function and plasma DHEAS was normal. Renal artery doppler did not reveal significant stenosis.
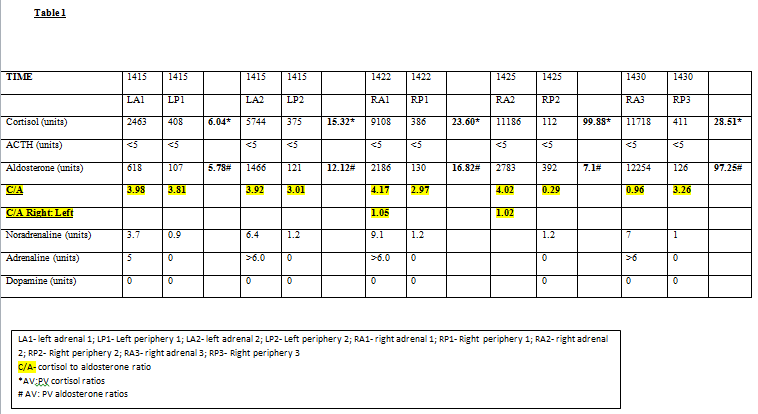
24 hour urine free cortisol measurements were 181nmol/L and 454nmol/L (n<350nmol/L). Her ACTH remained undetectable on numerous occasions (<5pg/ml). Due to difficulty in ceasing inhaled steroids an overnight 1mg Dexamethasone suppression test was performed whilst the patient was taking fluticasone/salmeterol. The following morning cortisol was 278 nmol/L (n<120nmol/L). Persistent hypercortisolism was then confirmed with IV dexamethasone suppression testing1 performed after withholding inhaled fluticasone for 3 days. An Adrenal CT scan showed a slightly enlarged left adrenal with an 8mm nodule at the inferior pole (Hounsfield unit <5). Given the lack of localisation of cortisol secretion on anatomical imaging functional imaging with iodocholesterol was performed but also non-diagnostic. Adrenal vein sampling was thus performed2, 3 (Table 1). Results were consistent with bilateral autonomous cortisol secretion. The patient was subsequently referred for bilateral adrenalectomies.
The case discussion evaluates the challenges of diagnosing hypercortisolism when exogenous steroids cannot be ceased, the importance of selecting an assay that would reliably exclude cross reacting steroids and methods in localising the source of cortisol secretion when conventional imaging is unhelpful. Histology results will be available by the conference date.
- 1. Jung C, Alford FP, Topliss DJ, Burgess JR, Long F, Gome JJ, Stockigt JR, Inder WJ. The 4-mg intravenous dexamethasone suppression test in the diagnosis of Cushing's syndrome. Clin Endocrinol (Oxf). 2010 Jul;73(1):78-84
- 2. Doppman JL, Gill JR Jr. Hyperaldosteronism: sampling the adrenal veins. Radiology. 1996; 198:309–312
- 3. Young WF, du Plessis H, Thompson GB, Grant CS, Farley DR, Richards ML, et al. The clinical conundrum of corticotropin-independent autonomous cortisol secretion in patients with bilateral adrenal masses. World J Surg. 2008;32(5):856-62