Poster Presentation The Annual Scientific Meeting of the Endocrine Society of Australia and the Society for Reproductive Biology 2014
Osteoporosis management at Western Health - a retrospective audit (#239)
Objectives:
To compare osteoporosis management among different units at Western Health with previously published “best-practice” guidelines
To audit outcomes of patients presenting to Western Health with fragility fractures
To investigate patient factors influencing length of stay
Background:
Osteoporosis is frequently unrecognised and inadequately managed, despite availability of effective therapies. Anecdotal experience suggests that significant variation in osteoporosis management exists among different units.
Methods:
A retrospective audit of Western health patients ≥60 years of age, presenting with fragility fractures1 from July to December 2012, was performed. Admission episodes were identified using the keyword “fracture” under the ICD-10 coding system. Electronic Medical Records were reviewed by one investigator to identify fragility fractures. Demographic information, documentation of existing osteoporosis treatment, risk factors, investigations, and interventions on discharge were collected and entered into a standardized database.
Results:
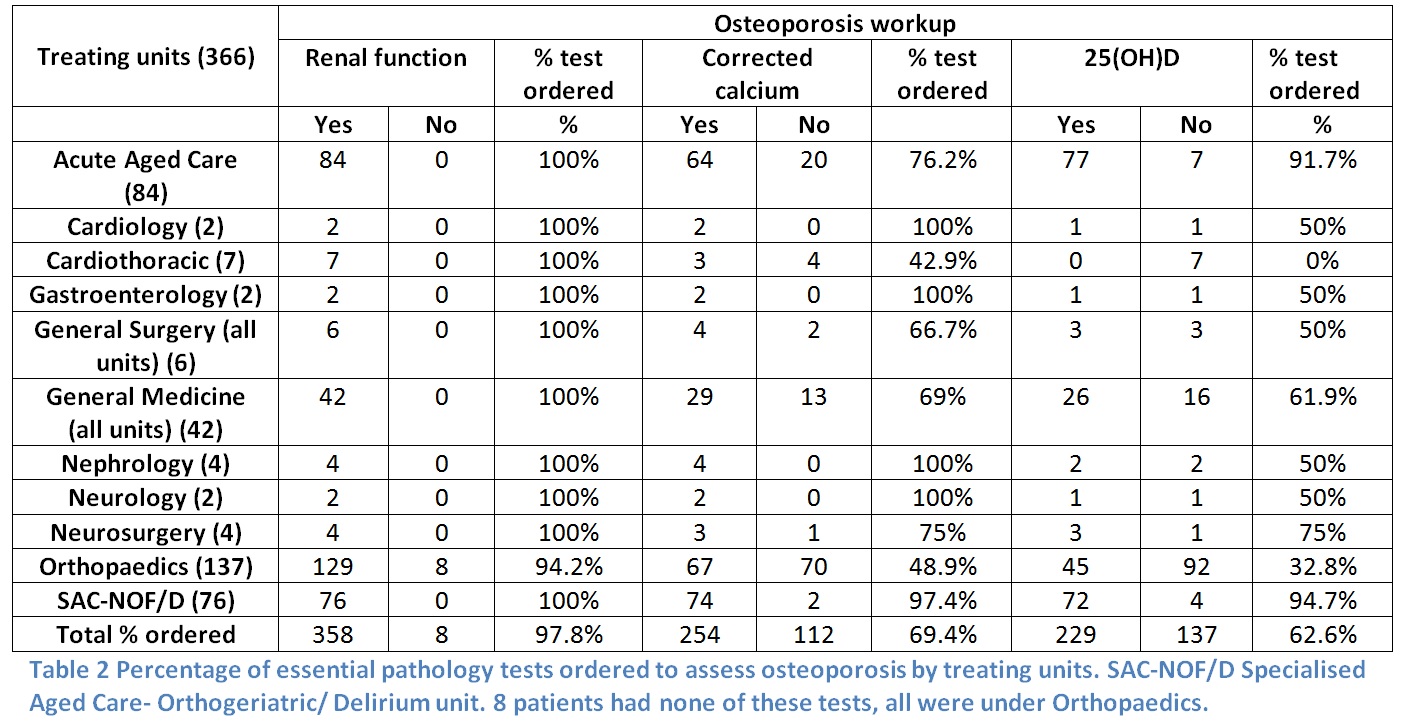
366 fragility fracture admissions were included. 31.1% had documentation regarding the presence of osteoporosis/osteopenia. Only 5.5% had documentation of a prior bone mineral density (BMD) scan. 56.3% had renal function, serum 25(OH)D and calcium tested, with the worst performance by Orthopaedic and Cardiothoracic units. 1.9% of admitted patients had inpatient BMD scans, and 4.6% had a scan organised upon discharge. 40% were not taking osteoporosis therapies prior to admission; only 15.6% of these patients were initiated on ≥1 osteoporosis therapies on discharge. Of patients discharged from acute units, 9.3% were on triple therapy2; 35.8% were discharged on no treatment. At hospital discharge 6.6% were deceased, 10.4% were non-ambulant, and 66.4% required assistance with mobility. The only patient factor influencing length of stay was fracture type (hip>wrist, foot and hand).
Conclusion:
Significant variation in osteoporosis management exists between units at Western Health, with low investigation and treatment rates. A systematic approach, such as a fracture liaison service, is required to improve these outcomes.